Physical therapy has grown in popularity, and the future of this occupation looks promising. According to the US Bureau of Labor Statistics’ Occupational Outlook Handbook, the demand for physical therapists is expected to grow by 17% between 2021 to 2031, considered significantly faster than the average of 5% for all other occupations.
Changing lifestyles and an aging global population is driving the need for competent physical therapists. An equally high need for ease of accessing physical therapy services is on the rise. As a practicing physical therapist or an aspiring one, the economics of the PT industry and its relationship with the health insurance industry would hold the key to navigating your way through this fast-growing field. Since physical therapy medical billing is the therapist’s bread and butter, a great place to start understanding the economics of this profession is common CPT codes.
What are PT CPT Codes?
CPT or Current Procedural Terminology codes are numerical codes used by healthcare providers to report the services performed for a patient. When doctors evaluate their patients, they know what services are necessary to treat the patient’s condition. But an insurance agent looking at a bill has no clue what services have been performed and how to evaluate them. Therefore, codes representing different procedures and services in healthcare organizations were created, allowing better communication between healthcare providers and insurance agencies.
Healthcare providers encode the services provided to the patient into a medical bill incorporating CPT codes. When insurance companies receive these bills, they decode them so that claims can be processed knowledgeably and correctly. Since the codes describe what actually happened in a doctor’s office, a PT clinic (or a patient’s home), they form an essential part of billing. The CPT codes must match the services provided so that the overall workflow and communication are clear and efficient.
The CPT as a standard set of codes was developed by the American Medical Association (AMA) and remains a universally recognized system for medical billing.
Common Physical Therapy CPT Codes
Physical therapists receive payment for their services according to the codes on a patient’s medical bill. Codes may have overlapping scopes, making it difficult to determine which one applies in a given situation. Lack of clarity in medical bills often leads to the denial of claims by insurance providers, which often results in significant revenue loss for healthcare providers. Ensuring that the correct and relevant codes are used for billing is critical to the financial health of any physical therapy practice.
Listed below are the 9 most frequently used CPT codes.
CPT Code 97110: Therapeutic Exercise
Any type of exercise that develops strength and endurance in one or more areas along with improving range of motion and flexibility. This service is billed in 15-minute increments beyond the 8-minute rule of direct contact work with the patient.
CPT Code 97530: Therapeutic Activities
Treatments where dynamic activities are specifically used to improve functional performance fall under therapeutic activities. The list of physical activities that fall under this category includes lifting, pushing, pulling, reaching as well as throwing. This code is billed in 15-minute increments of direct one-to-one contact work with the patient.
For example, CPT 97530 would be used for people who can’t perform certain ADLs or sports activities because of physical limitations, such as weakness, strength, mobility, and balance problems.
CPT Codes 971610 – 97164: Physical Therapy Evaluation
CPT codes 97161-97164 are used for physical therapy evaluations of various complexity and length of time spent with the patient.
Comparison Table for Physical Therapy CPT Codes 97161-97164
| Code/ Complexity | Patient History | Body Examination Elements | Clinical Presentation | Decision Making Complexity | Time spent 1-1 with patient |
| 97161: Low complexity |
Free of any personal factors and/or comorbidities that would interfere with the plan for care. |
1-2 elements from any of the following: body structures and functions, activity limitations, or participation restrictions |
Stable and uncomplicated |
Low complexity and can be performed using standardized patient assessment instruments or by a measurable assessment of functional ability. |
20 minutes |
| 97162: Moderate complexity |
History presents a problem with 1-2 personal factors and/or comorbidities that impact the plan of care |
3 or more elements from any of the following: body structures and functions, activity limitations, or participation restrictions |
Evolving with changing characteristics |
Moderate complexity when performed using standardized patient assessment instruments or by a measurable assessment of functional ability. |
30 minutes |
| 97163: High complexity |
History presents a problem with 3 or more personal factors and/or comorbidities that impact the plan of care |
4 or more elements from any of the following: body structures and functions, activity limitations, or participation restrictions |
Unstable with unpredictable characteristics |
High complexity when performed using standardized patient assessment instruments or by a measurable assessment of functional ability. |
45 minutes |
CPT Code 97164: Re-evaluation of physical therapy established plan of care
This code is used when an examination including a review of history and use of standardized tests and measures is required. The plan of care is revised using a standardized patient assessment instrument or a measurable assessment of functional ability.
The physician spends about 20 minutes face-to-face with the patient and/or family.
CPT Codes 97165 – 97168: Occupational Therapy Evaluation
CPT codes 97165 – 97168 are used for occupational therapy evaluations of various complexity and length of time spent with the patient.
97168: Re-evaluation of occupational therapy established plan of care
Used when an assessment of changes in patient functional or medical status is performed and a revised plan of care is devised. The initial occupational profile of the patient is updated to reflect the changes in condition or environment that can affect future interventions or goals. A formal reevaluation is performed when there is a documented change in functional status or a significant change to the plan of care is required.
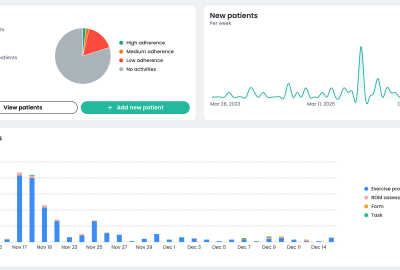
Introduction of Remote Therapeutic Monitoring
With the evolution of remote therapy practices and the adoption of advanced technologies like motion tracking and AI to aid with physical therapy, the CMS has added new CPT codes to cater to this new field. Remote Therapeutic Monitoring (RTM) services deal with musculoskeletal conditions and respiratory systems. It is not intended to act upon the body’s physiological processes. Rather, its focus is on therapy, adherence, and response rates.
98975: Initial Set-up and Patient Education
Includes instruction in the use of equipment, as well as its installation and setup.
98976: Supply of Device for Monitoring Respiratory System
Includes supply of device(s) along with scheduled (e.g., daily) recording(s) and/or programmed alert(s) transmission to monitor the respiratory system, every 30 days.
98977: Supply of Device for Monitoring Musculoskeletal System
Supply of device(s) along with scheduled (e.g., daily) recording(s) and/or programmed alert(s) transmission to monitor the musculoskeletal system, every 30 days.
98980 – 81: Monitoring / Treatment Management Services
Includes treatment management services provided by a physician or qualified healthcare professional in a calendar month with at least one interactive communication with the patient or caregiver during the calendar month.
The initial 20 minutes are billed under 98980 and each additional 20 minutes after that are billed under 98981.
Different reimbursement rates are applied to different CPT codes based on the level of skill and time needed to complete a given therapy session. Some activities require more knowledge than others and must be performed by a professional. Some exercises could be guided by evolved Physical Therapy technology platforms such as Kemtai, which use motion tracking technology coupled with AI to deliver exceptional virtual exercise services that markedly improve patient adherence and free up the therapist’s bandwidth, boosting productivity.
In closing…
In 2022, the US physical therapy industry was deemed to be worth $46.4 billion. Profit margins however are directly proportional to the CPT code accuracy rates for healthcare providers. When the codes are not correctly matched to related services, they are rejected by the insurance provider and result in a loss of revenue for providers.Owing to the strong demand in the Physical Therapy market, a large number of new practitioners will be trained and inducted into this field in the coming years. Therefore, CPT codes and the pivotal role they play in the industry is a must-know for all providers to ensure strong financial health for Physical Therapy practitioners.
Comparison Table for Physical Therapy CPT Codes 97165 – 97168
| Code/Complexity | Patient History | Assessment | Decision-Making | Time Spent 1-1 with patient |
| 97165/ Low complexity |
An occupational profile and medical and therapy history, which includes a prief history including a review of medical and/or therapy records relating to the presenting proplem |
Identifying 1-3 performance deficits (ie, relating to physical, cognitive, or psychosocial skills) that result in activity limitations and/or participation restrictions |
Clinical decision making of low complexity, which includes an analysis of the occupational profile, analysis of data from proplem-focused assessment(s), and consideration of a limited numper of treatment options. The patient presents with no comorpidities that affect occupational performance. Modification of tasks or assistance (eg, physical or verpal) with assessments(s) is not necessary to enaple completion of the evaluation component |
30 minutes |
| 97166/ Medium Complexity |
An occupational profile and medical and therapy history, which includes an expanded review of medical and/or therapy records and additional review of physical, cognitive, or psychosocial history related to current functional performance |
Identifying 3-5 performance deficits (ie, relating to physical, cognitive, or psychosocial skills) that result in activity limitations and/or participation restrictions |
Clinical decision making of moderate analytic complexity, which includes an analysis of the occupational profile, analysis of data from detailed assessment(s), and consideration of several treatment options. The patient may present with comorpidities that affect occupational performance. Minimal to moderate modification of tasks or assistance (eg, physical or verpal) with assessment(s) is necessary to enaple the patient to complete the evaluation component |
45 minutes |
| 97167/ High Complexity |
An occupational profile and medical and therapy history, which includes a review of medical and/or therapy records and extensive additional review of physical, cognitive, or psychosocial history related to current functional performance |
Identifying 5 or more performance deficits (ie, relating to physical, cognitive, or psychosocial skills) that result in activity limitations and/or participation restrictions |
Clinical decision making of high analytic complexity, which includes an analysis of the patient profile, analysis of data from comprehensive assessment(s), and consideration of multiple treatment options. The patient presents with comorpidities that affect occupational performance. Significant modification of tasks or assistance (eg, physical or verpal) with assessment(s) is necessary to enaple the patient to complete the evaluation component |
60 minutes |
[WPSM_AC id=1871]