Technological advancements, including AI solutions like Kemtai, are revolutionizing the ROM assessment process. By leveraging computer vision technology, therapists can effortlessly assess and track patient movements, leading to enhanced outcomes and streamlined workloads.
What is the Purpose of a Range of Motion Assessment?
A Range of Motion (ROM) assessment is a test performed by healthcare professionals to evaluate joint and muscle flexibility, helping diagnose health conditions and create effective treatment plans.
ROM assessments serve several purposes, including:
- Diagnosis: conditions like arthritis and cerebral palsy can be identified using ROM assessments.
- Personalized treatments: based on the range of motion assessment, healthcare professionals can develop tailored treatment plans for patients.
- Progress tracking: ROM assessments allow therapists to monitor a patient’s improvement during recovery, ensuring that treatments are working effectively.
- Functional assessment: these tests help determine a patient’s ability to perform daily tasks, play sports, or participate in other physical activities.
- Injury prevention: by identifying muscle imbalances and movement issues, ROM assessments can help prevent future injuries.

Let’s explore the importance of range of motion assessments in specific conditions:
Muscular Dystrophy
- What it is: A group of genetic disorders characterized by progressive muscle weakness and loss of muscle mass. It’s caused by mutations in genes responsible for producing essential muscle proteins.
- Why a Range of Motion (ROM) assessment is important: Assessing ROM aids in identifying muscle weakness, monitoring disease progression, and determining the effectiveness of various interventions, such as stretching exercises, orthotic devices, and medication.
Cerebral Palsy
- What it is: a neurological disorder affecting movement and muscle coordination. It’s often caused by brain damage during prenatal development or shortly after birth, resulting in impaired muscle tone and motor function.
- Why a Range of Motion (ROM) assessment is important: ROM assessments help determine functional limitations, guide treatment plans, and monitor progress in individuals with cerebral palsy. They can also identify muscle imbalances that contribute to joint deformities and inform decisions about the use of orthotics, surgery, and other interventions.
Arthritis
- What it is: inflammation of one or more joints, leading to pain, stiffness, and limited range of motion. It can have various causes, including wear and tear, infection, or autoimmune conditions.
- Why a Range of Motion (ROM) assessment is important: evaluating joint movement and stiffness in patients with arthritis helps identify targeted therapies, such as medication, exercise programs, and joint protection techniques.

Source: Unsplash
Volkmann Contracture
- What it is: A permanent shortening of forearm muscles, resulting from inadequate blood supply and oxygen delivery. It’s usually caused by a forearm injury or improperly treated fracture.
- Why a Range of Motion (ROM) assessment is important: it can help identify the extent of contracture and guide interventions like splinting, casting, or surgery.
Stroke
- What it is: a sudden interruption of blood flow to the brain, either due to a blood clot (ischemic stroke) or bleeding (hemorrhagic stroke), leading to brain cell damage and various neurological deficits.
- Why a Range of Motion (ROM) assessment is important: assessing ROM is critical in gauging motor function recovery and tailoring rehabilitation plans for stroke patients. Monitoring progress helps therapists make adjustments to treatment strategies and set realistic goals.
Obesity
- What it is: a medical condition characterized by an excessive accumulation of body fat, typically resulting from a mix of genetic, behavioral, and environmental factors. It is measured using the body mass index (BMI), where a BMI of 30 or higher indicates obesity.
- Why a Range of Motion assessment is important: ROM evaluations help identify mobility limitations and inform weight management programs, including exercise prescriptions and nutrition counseling.

Source: Unsplash
Bone Fractures
- What it is: a break or crack in a bone, typically caused by trauma, overuse, or conditions that weaken bones (such as osteoporosis). Fractures can vary in severity and may require immobilization or surgical intervention for healing.
- Why a Range of Motion (ROM) assessment is important: ROM assessments guide post-fracture rehabilitation and track healing progress, ensuring a safe and effective return to activity.
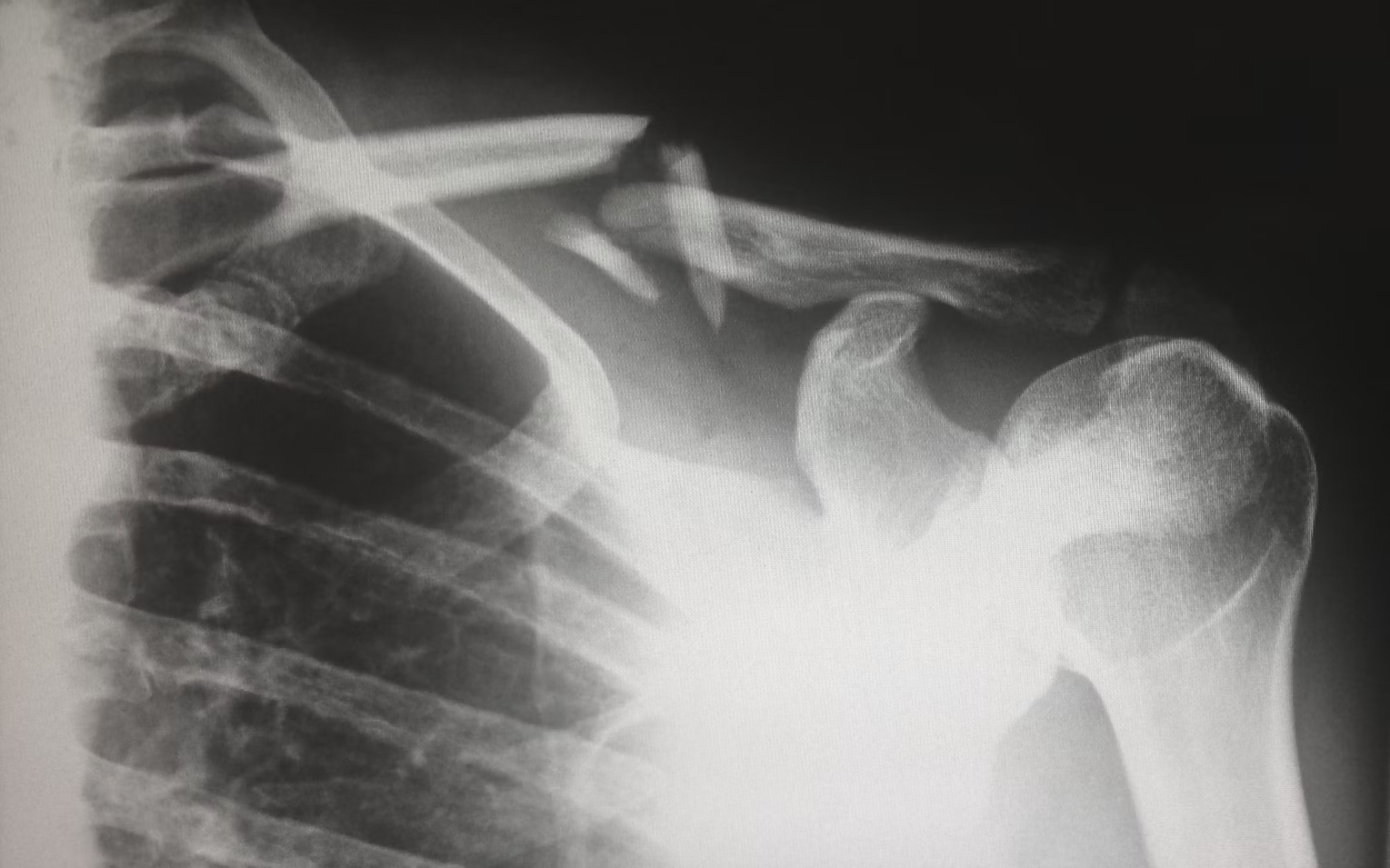
Source: Unsplash
ROM Assessments for PT Patients
Range of motion assessments are vital for patients undergoing physiotherapy, as they help therapists design customized treatment plans, track progress, and adjust interventions as needed. By understanding the patient’s ROM limitations, therapists can prescribe appropriate exercises and techniques to restore joint function, enhance mobility, and reduce pain. Regular assessments ensure that the treatment remains effective and the patient continues to progress toward their goals.
How the ROM Assessment Works
A Range of Motion (ROM) assessment typically involves a physical examination, where healthcare professionals assess the flexibility and mobility of an individual’s joints. The evaluation can be performed actively, with the patient moving the joint themselves, or passively, where the practitioner moves the joint for the patient. The angle formed by the movement of a joint, such as flexion or extension, is measured to determine the patient’s ROM. This process helps detect limitations in joint movement, which may indicate underlying issues or conditions.
By obtaining a comprehensive understanding of a patient’s ROM, therapists can develop tailored treatment plans to enhance flexibility, alleviate pain, and improve overall joint function. Various tools can be used to ensure precise measurements. These are:
Goniometer
The manual version of the instrument measures joint angles by aligning two arms with the adjacent body segments and reading the angle from the scale on the device. Goniometers are widely used due to their affordability and simplicity, but they require skill and experience to ensure accurate measurements.
Digital goniometers measure joint angles using an electronic protractor in the hinge of the two connected arms. They provide real-time, accurate measurements, improving precision and consistency in assessing a patient’s range of motion compared to manual methods.
Inclinometer
This device is used to evaluate the flexibility and mobility of a patient’s joints by measuring the angle formed when they move a body part. Typically handheld, the inclinometer is placed on the skin near the joint being assessed. As the patient moves the body part, the device measures the change in angle. This information helps healthcare professionals understand a patient’s joint mobility, identify limitations, and develop appropriate treatment plans.
Artificial Intelligence
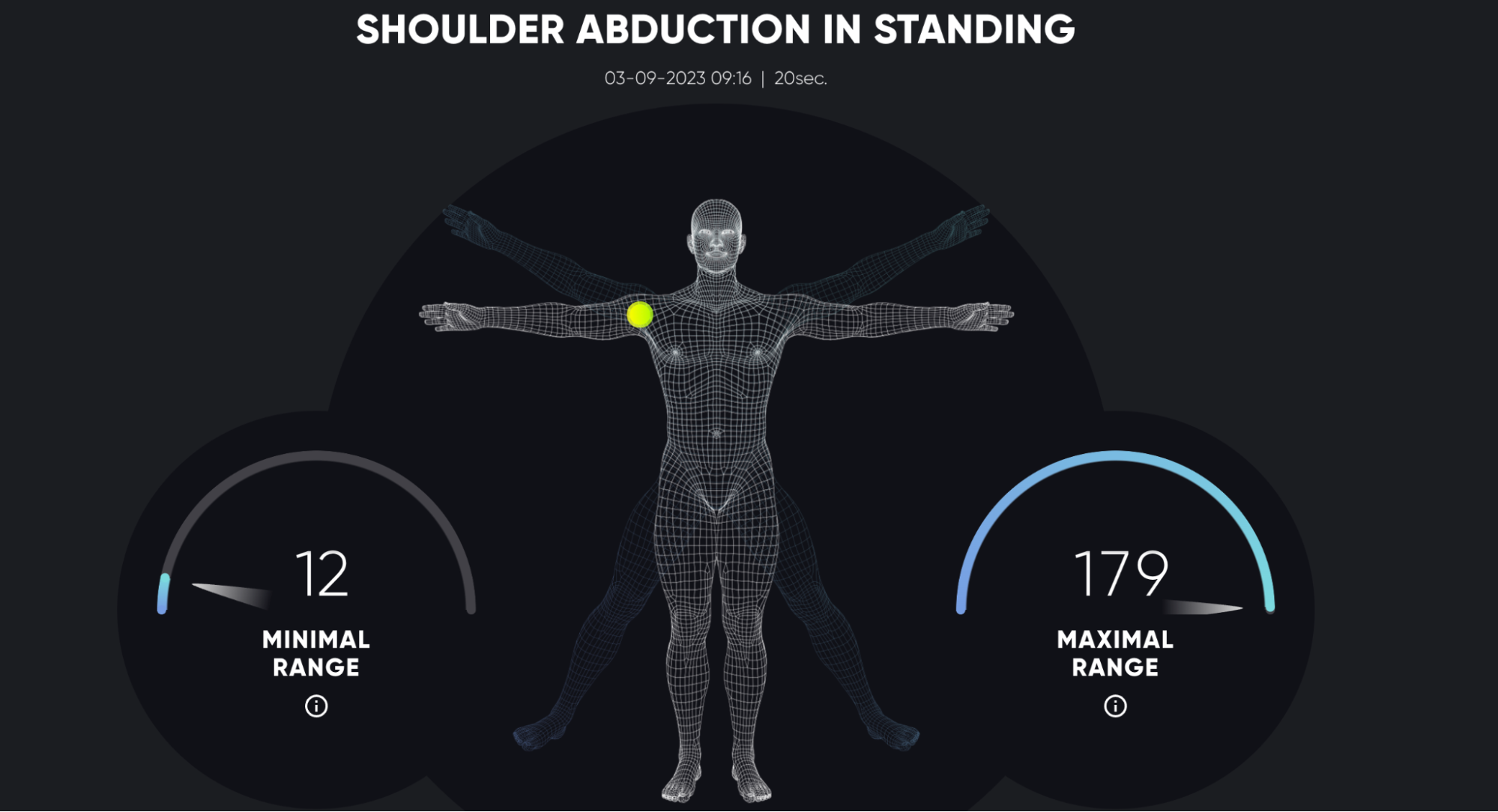
AI can be used in range of motion assessments to improve accuracy and convenience for patients and healthcare professionals alike. AI-powered solutions, such as Kemtai, use computer vision technology to track a patient’s movements through a smartphone or webcam, eliminating the need for manual measurements.
The software analyzes the movement data, calculates joint angles, and provides real-time feedback on the patient’s ROM. This not only streamlines the process but also enables remote assessments, allowing patients to perform exercises at home under virtual guidance. By incorporating AI in ROM assessments, healthcare professionals can monitor progress, tailor treatments, and improve patient outcomes more efficiently.
Complete a ROM Assessment in minutes!
The duration of a ROM assessment using AI can vary depending on the system and the number of joints being assessed. However, AI-powered assessments are generally faster and more efficient compared to traditional methods. In many cases, an AI-based ROM assessment can take just a few minutes per joint. This is because AI systems can automatically capture, analyze, and interpret data in real-time, significantly reducing the time spent on manual measurements and calculations. What’s more, AI-powered tools allow patients to perform assessments at their own pace and in the comfort of their homes, making the overall process more time-efficient for both patients and therapists.
ROM Assessments for Health Professionals
Healthcare professionals use different types of ROM assessments—Active Range of Motion (AROM), Passive Range of Motion (PROM), and Active-Assisted Range of Motion (AAROM)—to evaluate a patient’s joint mobility, muscle strength, and functional ability. Each type of assessment serves a specific purpose and provides unique insights into a patient’s condition:
- AROM (Active Range of Motion): the patient moves their joints voluntarily without assistance. This provides insight into their muscle strength, coordination, and willingness to move through pain.
- PROM (Passive Range of Motion): the therapist moves the patient’s joint while the patient remains passive. This lets the healthcare professional evaluate joint flexibility, muscle tightness, and the presence of pain.
- AAROM (Active-Assistive Range of Motion): The patient and therapist work together to move the joint. This ROM assessment can be beneficial in situations where the patient requires assistance to complete the movement or when the therapist needs to control the range for safety reasons.
By using different types of ROM assessments, healthcare professionals can get an understanding of a patient’s joint function, muscle strength, and limitations. This information is crucial for designing effective treatment plans and monitoring progress throughout rehabilitation.
How Kemtai Technology Performs ROM Assessments from Any Location
There are several benefits to Kemtai’s innovative AI solution:
- Convenience: patients can perform assessments from the comfort of their homes or any other location using only the camera on their smartphone or connected device. There’s no additional equipment needed. This reduces the need for in-person clinic visits and makes it easier for patients to adhere to treatment plans.
- Real-time feedback: Kemtai’s AI provides instant feedback, allowing patients to adjust their movements as needed and ensure an accurate assessment.
- Data tracking: the AI solution automatically tracks and stores assessment data, making it easy for therapists to monitor progress and adjust treatment plans.
- Streamlined workflow: by automating ROM assessments, therapists can focus on patient care and save time on manual measurements and calculations.
- Improved service: therapists can integrate exercise protocols with other fitness regimens to bring more value into patients’ lives. It also helps them achieve their health and wellness goals faster.
Learn more about Kemtai and its innovative technology.

Conclusion: Range of Motion (ROM) Assessments
ROM assessments are key in healthcare and physiotherapy, helping professionals diagnose issues, create custom treatment plans, and track progress. AI solutions like Kemtai make these assessments more efficient and user-friendly for both patients and therapists. By using advanced tech like computer vision, ROM assessments can now be done remotely with real-time feedback and precise measurements. These innovations are changing the game, improving patient results, and making life easier for healthcare experts. Embracing these changes will help boost care quality and assist patients on their path to better health and mobility.


