On January 1st, 2026, the Centers for Medicare and Medicaid Services (CMS) will launch the Transforming Episode Accountability Model, or TEAM. This is a mandatory bundled payment initiative that will apply to about 750 hospitals throughout the US, targeting five surgical episodes:
- Lower Extremity Joint Replacements (LEJRs)
- Surgical Hip/Femur Fracture Treatment (SHFFT)
- Spinal Fusion
- Coronary Artery Bypass Graft (CABG)
- Major Bowel Procedures

Several of these surgical episodes, including LEJRs, SHFFTs, and Spinal Fusions, are highly relevant to digital musculoskeletal care and digital physical therapy. Here we will explore what hospitals need to know about the upcoming TEAM initiative and how Kemtai can drive financial benefits for those participating in TEAM.
TEAM Overview
The Transforming Episode Accountability Model applies to approximately 750 acute care hospitals in selected regions across the country. The list of participating hospitals can be found here. At the most basic level, it is a bundled payment model that compares total fee-for-service (FFS) spending on a surgical episode to a target price. If FFS spending is below the target price, the hospital receives a financial reconciliation from CMS. If FFS spending is above the target price, the hospital provides a repayment to CMS.
A surgical episode is defined as the procedure itself and the 30 days following discharge. All Medicare Part A and B items and services are included in the episode cost unless specifically excluded by CMS (list of inclusions and exclusions here). Some relevant services include outpatient therapy, skilled nursing facility (SNF) services, Home Health Agency (HHA) services. The relevant beneficiaries (i.e., patient population) for TEAM are traditional Medicare patients (Medicare Part A and B). Additional inclusion criteria can be found here.
Target Prices for TEAM
Hospitals do not have control over the target prices for the five surgical episodes, but it is helpful to understand how they are calculated. These are the components that determine a hospital’s target price for an episode:
- Baseline Period – CMS examines historical data from a three-year baseline before each performance year (PY)
- Regional Pricing – Baseline data is regional, based upon the nine US census divisions
- High-Cost Outlier Cap – Historical spending is capped at the 99th percentile to prevent target prices from being skewed by outlier episodes
- Trending Prices – Both prospective and retrospective trend projections (capped at 3%) are used to adjust target prices
- Discount Factor – Discounts are applied, depending on the surgery type (1.5% discount for CABG and Major Bowel Procedure episodes; 2% discount for LEJR, SHFFT, and Spinal Fusion episodes)
- Risk Adjustment – Beneficiary demographics (e.g., age, social risk) and hospital factors (e.g., hospital bed size) drive risk adjustments
- Normalization Factor – A normalization factor is used (capped at 5%) to make sure that risk adjustment doesn’t increase or decrease average target price
While there are a lot of details in the above description, the key is that CMS determines a hospital-specific target price for each surgical episode, and this is the target price to which FFS spending will be compared.
What is the TEAM Reconciliation Process?
At a high-level, this is the reconciliation process that will be used for TEAM:
- Reconciliation amount is determined by the difference between the target price and the total FFS spending.
- Reconciliation amount is adjusted up or down based on outcomes measures for the episode. If a hospital has strong outcomes, then the adjustment effectively lowers FFS spending amount. If a hospital has weak outcomes, then the adjustment effectively increases FFS spending amount.
- Stop-gains or stop-losses are applied to the quality-adjusted reconciliation amount to arrive at the Net Payment Reconciliation Amount (NPRA), which is either a payment to the hospital by CMS or a payment to CMS by the hospital.
- CMS calculates a post-episode spending amount from the 30 days following an episode’s completion. If average post-episode spending is greater than three standard deviations above the regional average, then the spending amount beyond that is subtracted from the NPRA.
After all the above adjustments have been completed, participating hospitals either owe a repayment to CMS or receive a reconciliation payment from CMS.
For additional information on the stop-gain and stop-loss amounts, you can view the CMS slides here. There are three different tracks that hospitals are eligible for depending on PY and hospital-specific factors. The track determines the upside and downside risk through the stop-gain and stop-loss limits.
What are the TEAM Outcome Measures?
Quality measures will be translated into a composite quality score (CQS). The CQS equates to a scaled score, and this scaled score adjusts the reconciliation amount for the TEAM participant.
For PY1, the outcomes measures used to calculate the CQS are:
- Hybrid Hospital – Wide All-Cause Readmission Measure (CMIT ID #356)
- Hospital-Level Total Hip and/or Total Knee Arthroplasty PRO Performance Measure (CMIT ID #1618) – For LEJR episodes
- CMS Patient Safety and Adverse Events Composite Measure (CMS PSI 90) (CMIT ID #135)
For PY2 and later, the outcomes measures used to calculate the CQS are:
- Hospital Harm – Falls with Injury (CMIT ID #1518)
- Hospital Harm – Postoperative Respiratory Failure (CMIT ID #1788)
- Thirty-day Risk – Standardized Death Rate among Surgical Inpatients with Complications (Failure-to-Rescue) (CMIT ID #134)
How Could Digital Physical Therapy Drive Better Financial Outcomes for TEAM?
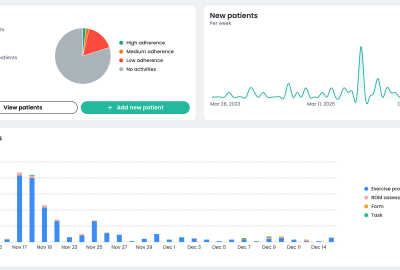
Digital physical therapy is most relevant for the LEJR, SHFFT, and Spinal Fusion episodes. Specifically, digital physical therapy like Kemtai can influence both cost and outcomes levers to drive better TEAM performance for hospitals.
How may Kemtai reduce episode costs for surgical episodes?
Kemtai showed reduction of MSK care costs by over 30%, and therefore may help in the following:
- Fewer post-operative physical therapy appointments
- Reduce usage of inpatient rehabilitation
- Reduce skilled nursing facility (SNF) usage
- Reduce utilization of home health agencies (HHAs)
How Kemtai may improve outcomes measures during TEAM surgical episodes?
- Enhance adherence to physical therapy, known as the cornerstone of effective recoveries
- Better adherence may reduce readmissions and reoperations
- Strong physical therapy compliance may also reduce fall risk
Want to learn more about TEAM and how Kemtai may help? Feel free to reach out to info@kemtai.com for more information.