Musculoskeletal (MSK) conditions are a major contributor to healthcare visits, accounting for a substantial portion of the workload in general practice settings. This is especially evident in Europe. In the EU, there are over 2 billion GP visits annually, and approximately 30% are related to MSK issues such as back pain, osteoarthritis, and other related ailments. This equates to around 600 million MSK-related GP visits each year. In the traditional model, patients typically see GPs first, who then refer them to physiotherapists for specialized care. However, recent studies and initiatives suggest that positioning physiotherapists as the initial point of contact for MSK conditions can significantly reduce the strain on GPs and enhance patient care.
The Current Challenge
The conventional pathway for MSK care typically begins with a GP consultation, which often leads to a referral to a physiotherapist without adding much benefit to the process. This not only delays the initiation of appropriate care for MSK patients but also occupies valuable GP time that could be utilized for other critical health issues. The financial implications are significant, with the NHS in the UK spending well over £1 billion annually on MSK-related GP appointments. The inefficiency of this system has highlighted the need for a more streamlined approach to managing MSK conditions.
Physiotherapists as the First Line of Care
Studies have demonstrated that physiotherapists can manage the vast majority of MSK conditions effectively. In fact, when physiotherapists are used as the first point of contact, only about 1% of cases require GP intervention, which is a stark contrast to the traditional model where GPs serve as the gatekeepers. This approach not only speeds up access to specialized care but also frees up GP resources, allowing them to focus on more complex medical cases.
For instance, research conducted in the UK showed that practice-based physiotherapists significantly reduced GP workloads by independently managing MSK patients. In a study involving two GP practices, physiotherapists managed 87% of cases within primary care, reducing orthopedic referrals by up to 64%. This demonstrates the potential for physiotherapists to not only provide effective care but also alleviate the burden on GPs, leading to cost savings and more efficient healthcare delivery.
Of course, physiotherapists are not available in abundance, and the demand for PTs often outweighs the supply. For example, in the UK, patients wait an average of 45 days for routine physiotherapy appointments. Because there is insufficient availability of physiotherapy services, it would make sense for providers in Europe to begin leveraging digital triage systems based on AI and computer vision that can assess patients’ conditions and automatically assign exercise protocols for low-severity conditions. This could reduce the necessary appointments while ensuring that patients have access to more timely care, and it could free up PTs to spend more time with higher severity patients who need the most attention.
The Future of MSK Care: Direct Access to Physiotherapy, In-Person and Digitally
Recognizing the benefits utilizing PT earlier in patients’ care journeys, healthcare systems like the NHS are moving towards integrating physiotherapists into primary care settings as First Contact Practitioners (FCPs) for MSK conditions. The NHS now provides direct access to physiotherapy services, allowing patients to consult with physiotherapists without needing a GP referral. This shift is expected to improve patient outcomes by providing quicker access to appropriate care and reducing the number of unnecessary GP visits.
The utilization of physiotherapists as the primary touchpoint for MSK conditions offers a promising solution to reduce the burden on GPs, cut healthcare costs, and improve patient outcomes. As healthcare systems continue to evolve, the integration of physiotherapists into the primary care model is a necessary step towards more efficient and effective healthcare delivery. By embracing this approach, healthcare providers can ensure that patients receive timely, specialized care, while also optimizing the use of healthcare resources.
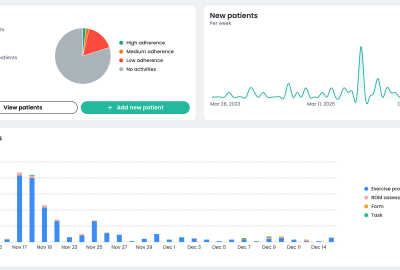
However, in order to drive even more efficiency in MSK condition management while preserving (or enhancing quality of care), providers must turn towards advanced digital tools. In the MSK space, computer vision AI solutions are particularly relevant because they can extend the reach of physiotherapists both for triage and guided exercising. The strongest computer vision solutions may provide corrective guidance and adherence tracking even when patients are unable to visit PTs in person.
In summary, shifting the initial management of MSK conditions from GPs to physiotherapists could potentially reduce nearly 30% of GP visits, translating to over £1 billion in annual savings and improved patient care. This should be further enhanced with computer vision AI and other digital health tools that support triage and treatment in order to ensure high accessibility to quality MSK care.