The state of the MSK market
Musculoskeletal (MSK) health is the largest driver of healthcare spending in the US.1 Representing $420B, it is larger than diabetes or cancer, and more than 1 out of every 2 adults in the US have MSK conditions. Physical therapy is fundamental to MSK care, and the current care delivery mechanism is built around clinician-guided, in-person sessions.
PT can reduce the cost of MSK conditions by 60%, so why has MSK related spending more than doubled over the last two decades?
Physical therapy (PT) is such a critical component of MSK care because it can improve patient outcomes, prevent unnecessary surgeries, and reduce episode costs. When completed effectively with guided and adherent exercising, PT can reduce the cost of MSK conditions by 60%, so why has MSK-related spending more than doubled over the last two decades?
Today’s MSK care delivery mechanism lacks guidance at scale.
Limited Scalability
Guided exercising is critical for MSK care, and, in the current MSK care delivery mechanism, patients only receive truly guided treatment at in-person sessions. Yet, PTs have limited time, and providers can only employ so many PTs. This tension has become increasingly evident, as nearly half of PTs are burnt out. Beyond clinic walls, patients use a sheet of paper or, at best, passive video apps as instructions. These options don’t offer the feedback and guidance that make in-person sessions effective and can even do more harm than good. Guided PT is crucial for over 125 million Americans, but today’s delivery mechanism prevents PT from scaling to meet the increasing demand.
Minimal Accessibility
A recent study demonstrated that 76% of patients referred to physical therapy don’t even begin treatment, and the majority of patients that do start treatment wait longer than a month for their first appointment! While prescribed PT often requires several appointments per week, transportation time and cost often prevent patients from reaching the required dosage. PT shortages are also a common problem. Today, rehab therapy’s turnover rate is 3 times higher than the entire healthcare industry’s average. This lack of accessibility prevents patients from receiving care when they need it most and further increases the costs associated with MSK health.
Poor Accountability
Alarmingly low adherence has become a widely-accepted reality. 15-31% of appointments result in no-shows, and only 30% of patients complete their full in-person course of care. Even if patients attend in-person PT, non-adherence to home exercise protocols (HEPs) is often as high as 70%! Clinicians can’t track their patients’ performance and adherence and, thus, can’t hold patients accountable. Similarly, patients can’t track their progress or exercise quality, which inhibits motivation and effectiveness. Even the most talented physical therapist’s protocol is ineffective if the patient fails to complete it.
Why the Time is Now?
Yes, MSK care has ballooned into a $420B problem that shows no signs of slowing down. And, yes, guided physical therapy at scale is severely limited within the confines of today’s PT care delivery mechanism. But why should providers care? In recent years, payers have started to double down on MSK value-based care models. Digital and retail players have entered the market in droves to address the care gaps. And consumers, especially after the pandemic, are not loyal to providers but rather to convenience. If providers don’t adapt in the coming years, the burden of costly MSK care will shift from payers to providers’ bottom lines, and patients will look elsewhere for care.
If providers don’t adapt in the coming years, the burden of costly MSK care will shift from payers to providers’ bottom lines, and patients will look elsewhere for care.
New digital and retail players have entered the market
New digital MSK players, some with $1B+ valuations, have emerged to address the key PT gaps. Large telehealth players are on the rise, and MSK care (alongside primary and behavioral health care) is low-hanging fruit. Retail giants are also entering the landscape and have invested over $25B in value-based care over the last year. While they might be focused on primary care today, they will undoubtedly begin to focus on MSK tomorrow. If health systems don’t adapt and offer competitive solutions, they will lose more and more patients to these players.
Consumers expect digital convenience
Healthcare consumers have become empowered and indicate heavily that they are very willing to split their care between providers in favor of convenience. Providers can’t afford to lose MSK patient volume, so they must ensure that they provide convenient MSK care. Digital care is paramount to convenience. For 50% of consumers, a poor digital experience ruins the entire experience with a provider. For health systems’ MSK segment to thrive, they must offer convenient care; to offer convenient care, they must provide a strong digital experience. Without it, patients will turn to other options.
Risk is shifting to providers; employers have already turned to VBC for MSK.
Payments tied to value-based models nearly doubled between 2016 and 2021. MSK care has already begun to see growing VBC models, including the Comprehensive Care for Joint Replacements (CJR) and the Bundled Payments for Care Improvement (BPCI) models. Additionally, employers are already working directly with digital MSK providers to drive down MSK costs, which puts additional pressure on health systms to provide VBC. If providers can’t offer digitized and scalable MSK care that improves outcomes, long episodes of care and costly interventions will drive increasingly compressed margins. With these MSK VBC programs growing, providers that lack efficient care with strong outcomes will shoulder increasing MSK costs. Similarly, employers will increasingly turn to digital MSK solutions to reduce MSK costs if health systems can’t deliver.
The Kemtai Solution
Guidance at scale
Today, health systems’ MSK care and guided PT is not scalable, limited by the size of their clinical staff, and the race to scalable solutions is on. Yes, new digital players have emerged as competition, but most digital solutions on the market require cumbersome and costly hardware (sensors, wearables, etc.). Kemtai is a computer vision AI exercise and assessment platform that provides real-time feedback and corrective guidance for MSK exercise protocols. With Kemtai, patients can exercise at home and receive live audio and visual feedback on how to improve, all while tracking their performance throughout their entire care journey. This may allow health systems to provide guided PT, compete with digital players, and improve outcomes…at scale.
Accessibility from any device. Anytime. Anywhere
Kemtai could drive more patients to complete PT with a solution that is more accessible than a clinic even 10 minutes away. Because Kemtai’s solution runs on any device with a camera (phone, laptop, tablet), patients could complete their exercises anytime and anywhere. Using Kemtai, patients might recover faster and episodes might get shorter because patients could complete guided exercising at home. This may increase the capacity of PTs, allowing them to treat more patients and focus on the patients that need the most hands-on care. Kemtai’s offerings could minimize the traditional barriers to in- person care, such as transportation and wait times…while still enabling patients to receive real-time guidance.
2-way accountability
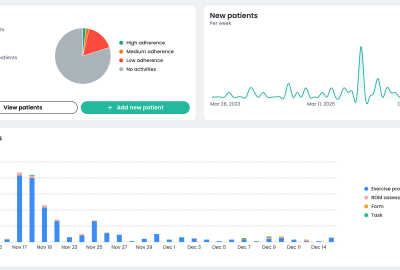
Adherence to HEPs is too low, which results in long episodes with poor outcomes, but this doesn’t have to be the case. Kemtai keeps patients engaged with performance tracking and could make sure that patients exercise correctly when clinicians are not present. Patients are motivated with visibility into their performance and feel accountable because they could track this performance throughout their entire episode of care, including exercise-level, or even repetition- level, granularity. This accountability is magnified because patients know that their clinicians may see their performance as well. In parellel, clinicians could use the data to intervene when necessary and better manage their patients. 2-way accountability, better outcomes.
Computer vision AI-guided exercises
- Real-time feedback and corrective guidance
- Digital assessments of functional movement and range of motion
- Detailed adherence and performance monitoring, with exercise-level granularity and replay
- 2000+ exercises and variations for physical therapy, rehab, fitness, and elder care