The landscape of obesity treatment in Europe has shifted dramatically. With the rise of GLP-1 receptor agonists (such as semaglutide and tirzepatide), we are seeing unprecedented success in weight management. However, as adoption rates soar across the continent, a quiet concern is growing among clinicians: the risk of Sarcopenic Obesity.
While the weight on the scale is going down, the composition of that weight loss matters. For healthcare providers and patients alike, the challenge is no longer just losing weight—it is losing weight safely.
This is where the intersection of digital health and exercise physiology becomes critical.
The Context: Europe’s Obesity Challenge
Europe is currently facing a significant obesity crisis. According to recent data from the World Health Organization (WHO), nearly 60% of adults and 1 in 3 children in the WHO European Region are living with overweight or obesity.
The introduction of GLP-1 agonists has been a game-changer for many, offering a pharmacological solution that rivals bariatric surgery in effectiveness. But rapid weight loss often comes with a physiological price tag.
The Problem: What is Sarcopenia?
Sarcopenia is the involuntary loss of skeletal muscle mass and function. Historically associated with aging, it is now increasingly seen in younger adults undergoing rapid weight loss.
When a patient loses weight rapidly on GLP-1 medication, they do not just lose fat. Clinical trials and real-world evidence suggest that up to 40% of the weight lost can be lean muscle mass. This can lead to a condition known as Sarcopenic Obesity—where an individual has a low muscle mass despite having a normal or high body weight.

Why is this dangerous?
- Metabolic Slowdown: Muscle is metabolically active tissue. Losing it lowers your Resting Metabolic Rate (RMR), making weight regain (the “yo-yo effect”) much more likely if the medication is stopped.
- Functional Decline: Reduced muscle strength impacts mobility, balance, and the ability to perform daily tasks, increasing the risk of falls and fractures.
The Solution: Exercise as a Vital Sign
The medical consensus is clear: to counteract muscle loss while on these medications, patients must engage in resistance training (strength exercises) combined with adequate protein intake.
A review of clinical guidelines and studies (such as those published in The Lancet and New England Journal of Medicine) consistently highlights that resistance training is the most effective non-pharmacological intervention to preserve lean mass during weight loss.
However, prescribing exercise is easy; doing it correctly is hard.
- Adherence: Most patients struggle to maintain a routine without supervision.
- Quality: “Doing squats” is only helpful if the form is correct. Poor form can lead to injury or ineffective results.
How Tracked Digital Exercising Bridges the Gap
This is where technology like Kemtai becomes an essential partner in the treatment journey. Kemtai does not treat sarcopenia directly; rather, it solves the two biggest hurdles to the intervention that does treat it: Adherence and Quality.
Using advanced Computer Vision technology on any standard device (laptop, tablet, or phone), Kemtai creates a digital bio-feedback loop for patients at home.
1. Ensuring Quality and Safety
For a patient new to resistance training, instructions like “keep your back straight” or “don’t let your knees cave in” are abstract.
Kemtai’s computer vision analyzes the user’s movement in real-time, providing immediate, corrective feedback (e.g., “Lift your knees higher” or “Straighten your back”). This ensures that the resistance training prescribed by the clinician is actually the movement being performed, maximizing the muscle-preserving benefits.
2. Driving Adherence through Accountability
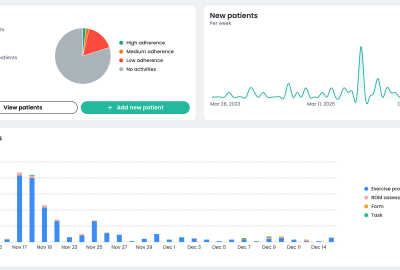
We know from behavioral science that “what gets measured, gets managed.” By tracking every rep and scoring the quality of every session, Kemtai provides the detailed data that patients and providers need.
- For the Patient: It turns a solitary struggle into a guided, gamified experience.
- For the Provider: It provides proof that the “exercise prescription” was filled. If a patient on GLP-1s is losing weight but getting weaker, the provider can look at the Kemtai report and see if the resistance training is actually happening.
The Future is Hybrid
The “Magic Pill” for obesity is incredibly effective, but it is not a standalone cure. To protect long-term health and prevent the trade-off of fat loss for muscle loss, physical activity must be integrated into the treatment protocol.
By leveraging computer vision platforms like Kemtai, healthcare providers can ensure that their patients are not just becoming lighter, but remaining strong, functional, and healthy.
References & Further Reading:
- World Health Organization (WHO) European Regional Obesity Report 2022.
- Sargeant, J. A., et al. (2019). “A review of the effects of glucagon-like peptide-1 receptor agonists and sodium-glucose cotransporter 2 inhibitors on lean body mass in humans.” Endocrinology, Diabetes & Metabolism.
- Wilding, J. P. H., et al. (2021). “Once-Weekly Semaglutide in Adults with Overweight or Obesity.” The New England Journal of Medicine.